A brief look
- It is estimated that 1 in 7 American adults (15% of the American adult population) have chronic kidney disease (CKD).
- To put this in perspective, 37 million Americans have CKD while just 21 million Americans have celiac or gluten sensitivity. Yet most grocers have not created a special section or aisle stocked with kidney-friendly foods as they have for gluten-free items.
- Those with advanced CKD have to watch their diet closely to prevent the condition from worsening.
- People with CKD must limit their intake of sodium, potassium, and phosphorus.
- Phosphorus in particular is often the most difficult to control. With the increased use of phosphate additives (e.g., sodium phosphate, calcium phosphate) in packaged goods, even foods typically considered low-phosphorus may have a high phosphorus content due to these additives.
- Kidney-friendly options for packaged goods are scarce, making grocery shopping a difficult experience for people with CKD.
- Of the packaged goods available in the market, certain categories have few kidney-friendly options, representing less than 15% of the total products in the category.
Dive deeper
Approximately 37 million Americans are affected by chronic kidney disease (CKD) which is a disease that is described as the gradual loss of kidney function. The two main causes are diabetes and high blood pressure. Those with CKD have to control their diet to prevent the disease from progressing further as it may eventually lead to kidney failure, and in the worst-case scenario, death.
People with CKD have reduced kidney function, thus the organ has a difficult time filtering out certain minerals such as sodium, phosphorus, and potassium. This could lead to a build-up of these minerals in a person’s bloodstream, eventually making them feel sick. Hence, foods that are high in sodium, phosphorus, or potassium must be avoided. This limits their diet substantially and makes every trip to the grocery store a headache-inducing experience.
Considering that 37 million Americans have this disease, and only 21 million Americans suffer from either gluten sensitivity or celiac, it’s surprising that grocers are not yet catering to this large market segment. For those who avoid gluten, stores all over America have gluten-free sections/aisles or ways to denote which products are gluten-free. This problem isn’t limited to just brick-and-mortar stores. Many of the top grocery websites and apps provide consumers with a gluten-free filter when searching for products. Meanwhile, those with CKD still have to scrutinize every individual product, whether in stores or online, to find kidney-friendly options.
To put into perspective how hard it is to find a product that is kidney-friendly, we looked at the majority of packaged products available in major US grocery stores via the Pinto database. By looking at the nutrition label values and the ingredients, we found that there were categories in which the percentage of kidney-friendly options available were below 15%.
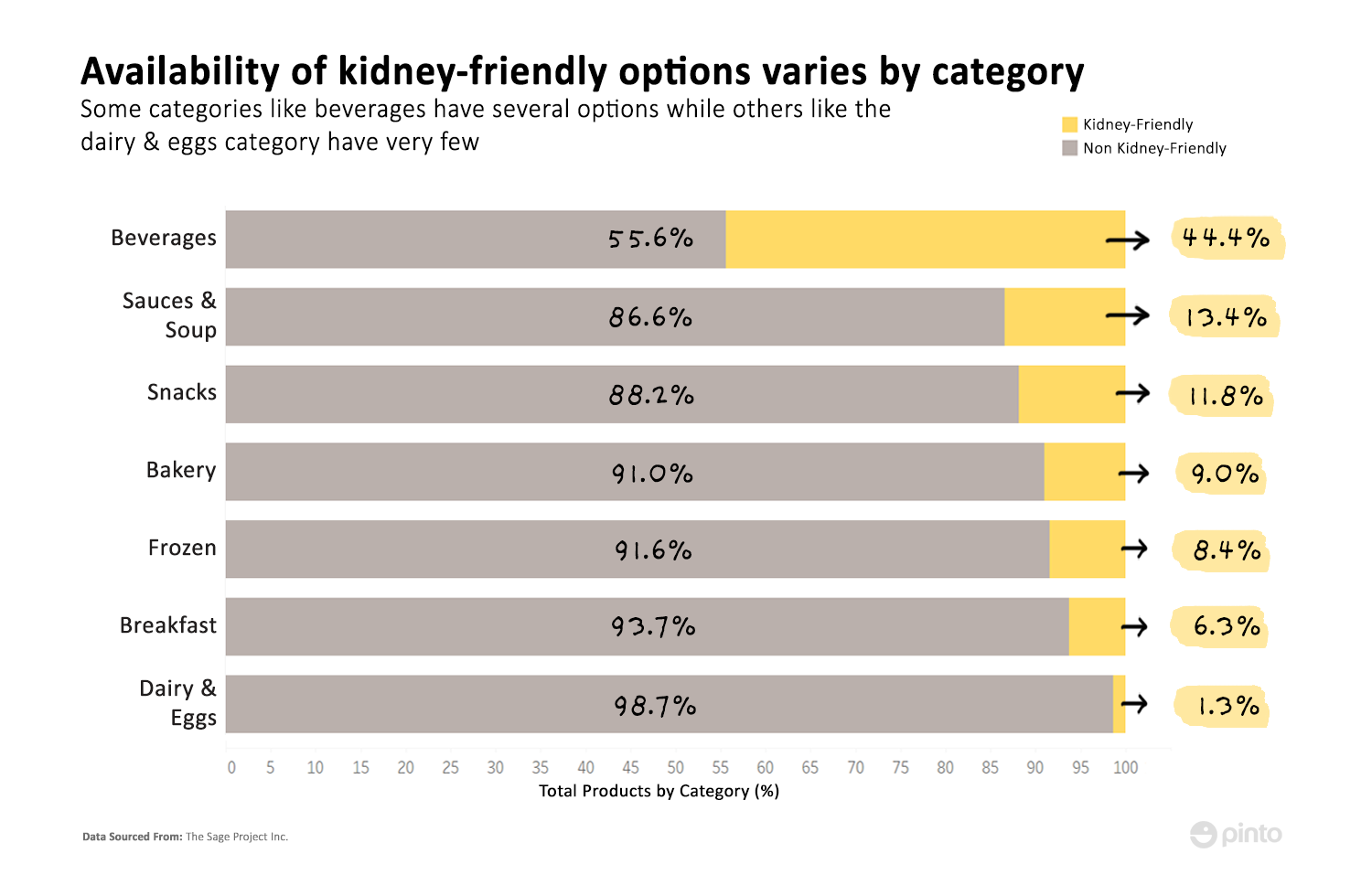
One reason for the low numbers is that the kidney-friendly diet is quite restrictive. Aside from sodium, phosphorus, and potassium, people with CKD have to avoid foods that are high in protein and fats as well. Thus, general healthy eating guidelines may not necessarily apply to them. Products such as avocados, beans, oatmeal, and certain nuts and grains that are generally considered healthy foods or snacks are not recommended for people with CKD.
Aside from sodium, phosphorus, and potassium, people with CKD have to avoid foods that are high in protein and fats as well.
When buying packaged goods, CKD patients often have to go through the arduous process of reading the fine print on nutrition labels to try and figure out if the product is kidney-friendly. However, that approach also has limitations because some nutrition labels do not report every mineral and nutrient.
Even fewer options are available in some sub-categories
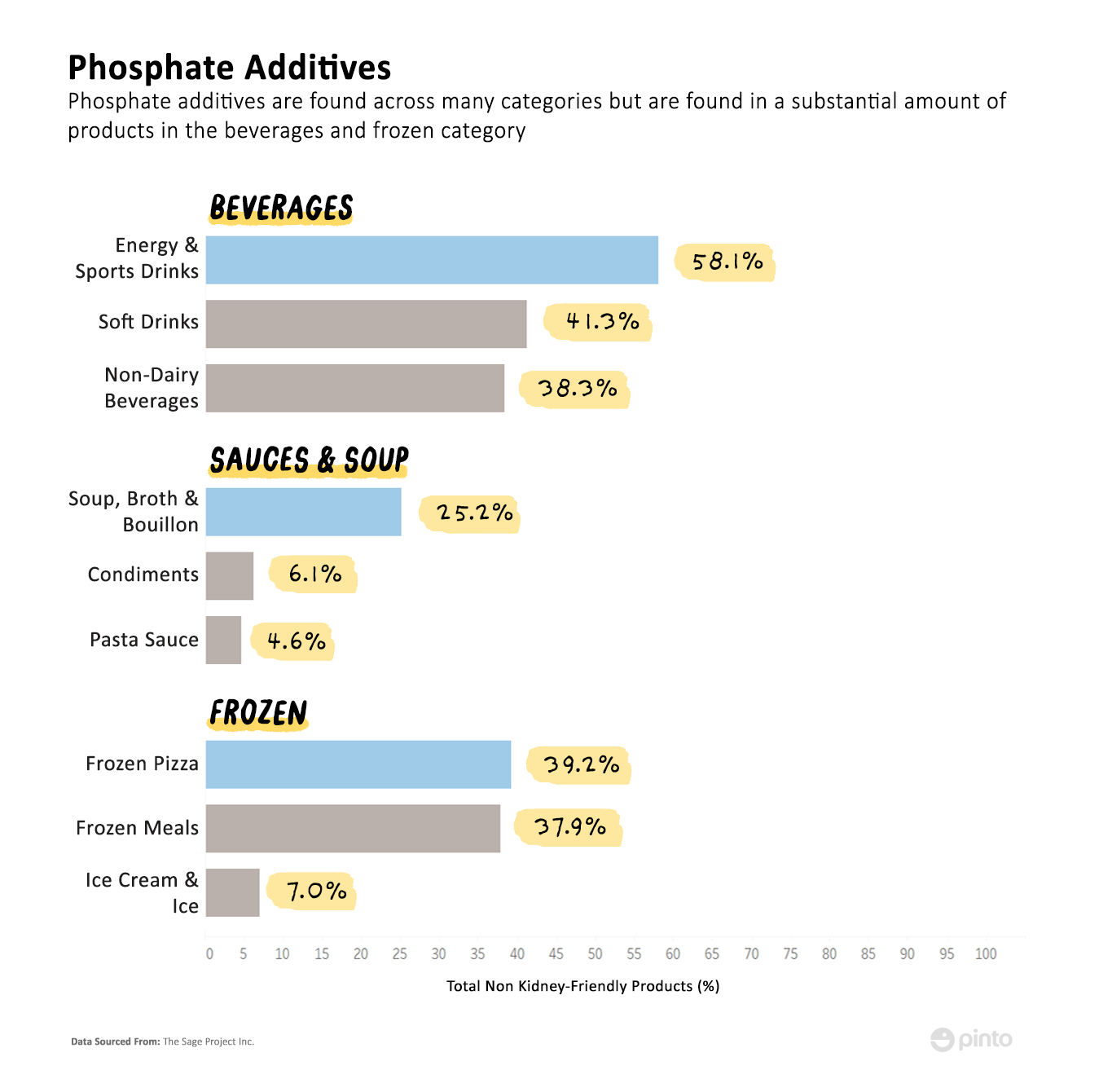
As we delve into sub-categories of kidney-friendly products, the picture gets more complicated. Some sub-categories have even fewer options than their top-level categories. Here, we picked some top-level categories that people with CKD tend to struggle with the most. These are categories such as: beverages, sauces & soup and frozen goods. In fact, we found that in some of the sub-categories, fewer than 10% of the available products are kidney-friendly.
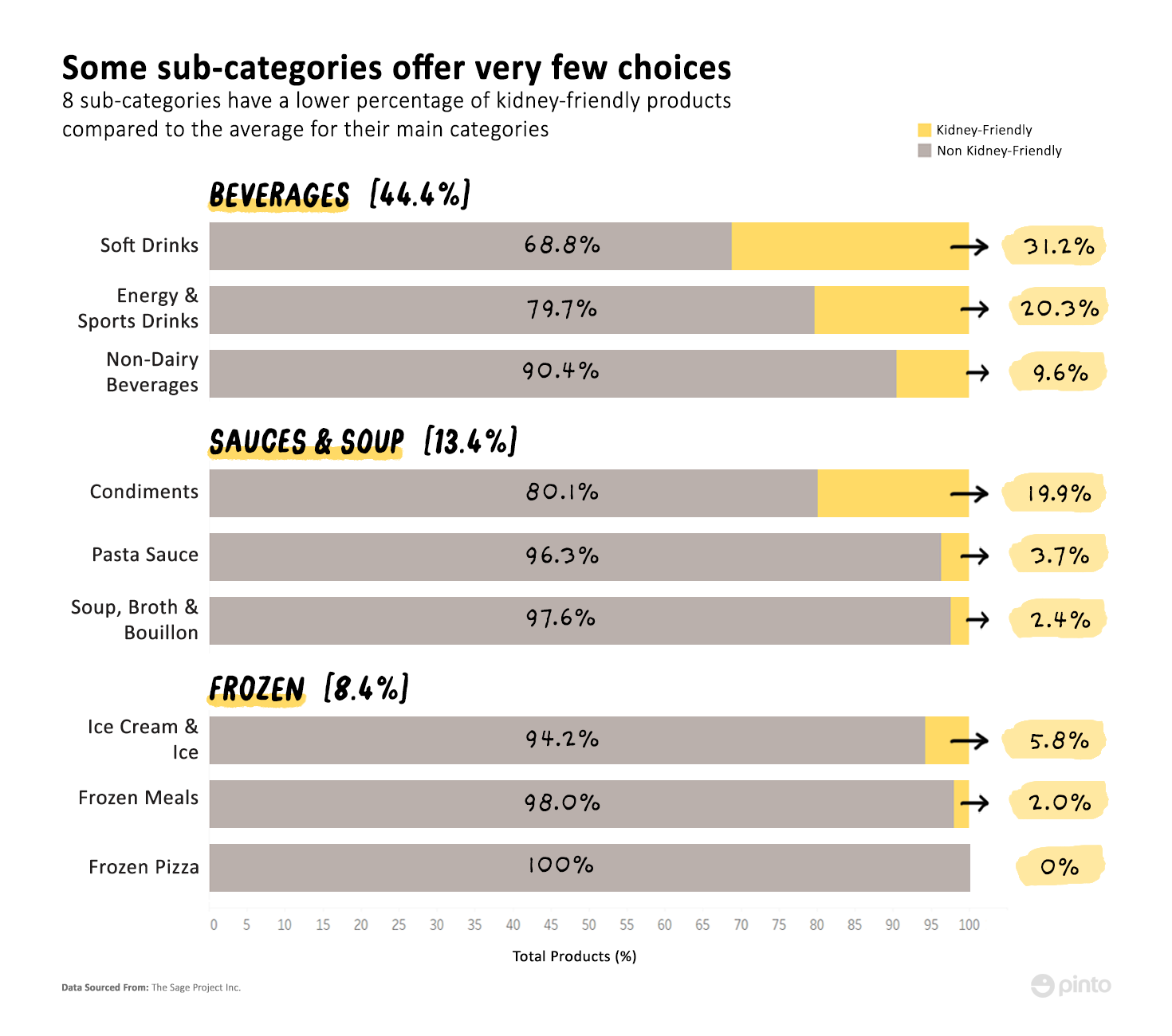
Though the overall beverages category performs fairly well with over 44% of the products being kidney-friendly, the graph above shows that this number discounts the fact that sub-categories such as non-dairy beverages (a sub-category that has been garnering a lot of public attention) have markedly fewer products that are kidney-friendly compared to the beverage category as a whole.
Other categories such as soup, broth & bouillon as well as frozen meals, have only a handful of products that qualify. Moreover, there are no frozen pizzas on the market that could be considered kidney-friendly.
Figuring out if a product is kidney-friendly can be quite difficult. While it’s easy to spot foods that are high in protein and fat, labels may not always accurately identify the amount of sodium, phosphorus, and potassium in a product. Those with CKD have to ensure that the foods they pick do not have sodium, potassium, or phosphorus levels that exceed those recommended by their dietitians.
New labels still don’t make it easy to spot phosphorus
Before the most recent update to labeling requirements, only sodium had to be reported on the nutrition label. However, with the FDA’s introduction of the new nutrition label (which is supposed to go into effect in 2020), potassium now has to be reported on the label too. However, figuring out the amount of phosphorus in products is still problematic.
Patients often find it difficult to control their phosphorus intake, and this is due in part to the fact that phosphorus is not listed on the nutrition label. To see how ubiquitous the mineral is, we took a look at the non-kidney-friendly products to see how many of them either contained a high-phosphorus ingredient or had higher than recommended amounts of phosphorus.
Data showed that for seven subcategories, those types of products accounted for over 60% of the non kidney-friendly products.

High-phosphorus foods can be found across all categories. Milk and dairy products are often high in phosphorus, which means that many foods that contain milk or dairy are also not kidney-friendly. This includes ice cream and many soups (especially creamy soups). Other examples include meat and seafood, beans, as well as certain nuts and grains, all of which can be found in many frozen foods.
Usually, CKD patients are given a guideline by their dietitians so they know which foods to avoid, and which ones they can consume. However, even if they were to follow these guidelines and look for products only containing low phosphorus foods, they can still end up consuming more phosphorus than the recommended threshold and this is because of phosphate additives.
Phosphate additives are difficult to avoid
Phosphate additives are compounds derived from phosphorus, such as sodium phosphate and calcium phosphate, that are often added to packaged goods for a number of reasons. The additives are used for leavening, enhancing flavor and color, balancing acidity, and preventing spoilage. Obviously, the additives perform important functions, but they also increase the phosphorus content of a product.
Phosphate additives are especially prevalent in beverages as well as frozen meals and pizza. Our data shows that for those sub-categories, over 35% of the non-kidney-friendly products contain phosphate additives.
When the nutrient label does not report a phosphorus value, CKD patients have no choice but to avoid products that contain phosphorus additives, even if the phosphorus content may not exceed the allowed threshold.
Most companies choose not to report the phosphorus value because it can be difficult to calculate accurately. This is because phosphates can be classified in two different ways: organic and inorganic. Organic phosphate is naturally found in foods while inorganic phosphate refers to ingredients such as phosphate additives.
The problem here is that inorganic phosphate is more bio-available than organic phosphate. This means that the body can absorb inorganic phosphate more readily, absorbing 90% to 100% of it versus organic phosphate, which is absorbed at rates of 40% to 60%. Thus, to arrive at the true phosphorus value for a product, one would have to differentiate between an organic and inorganic phosphate source and perform the necessary calculations.
The body can absorb inorganic phosphate more readily, absorbing 90% to 100% of it versus organic phosphate, which is absorbed at rates of 40% to 60%.
Considering that it is not mandatory to report the phosphorus value, most companies choose not to go through all that trouble.
Kidney-friendly displays would appeal to this large market segment
Grocers have an opportunity to boost their business while also making the shopping experience much better for those with CKD. Grocers should consider setting up a section or aisle exclusively for pre-screened kidney-friendly products. In addition, providing a kidney-friendly search filter on their online platform can help create a simpler experience for people with kidney disease.
Unfortunately, identifying kidney-friendly products is not as easy as it should be. While there are established processes and official bodies for certifying products as gluten-free or low FODMAP, there is no such system in place for kidney-friendly products. Grocers will have to do some of the legwork to decipher nutrition labels and consult with dietitians to determine the suitability of products for those with CKD.
Ten years ago, very few grocery stores or restaurants had gluten-free options. Gradually, the food and grocery industry started to respond to consumers’ growing demand for gluten-free products. Now, gluten-free aisles are commonplace. The 37 million Americans with chronic kidney disease will no doubt flock to places that offer them a hassle-free shopping experience.